PERIODONTAL TREATMENT IN CHICO
What is periodontitis?
Periodontitis is a serious infection of the gums. It’s caused by bacteria that have been allowed to accumulate on your teeth and gums. As periodontitis progresses, your bones and teeth can be damaged. However, if periodontitis is treated early and proper oral hygiene is maintained, the damage can be stopped.
What are the stages of periodontitis?
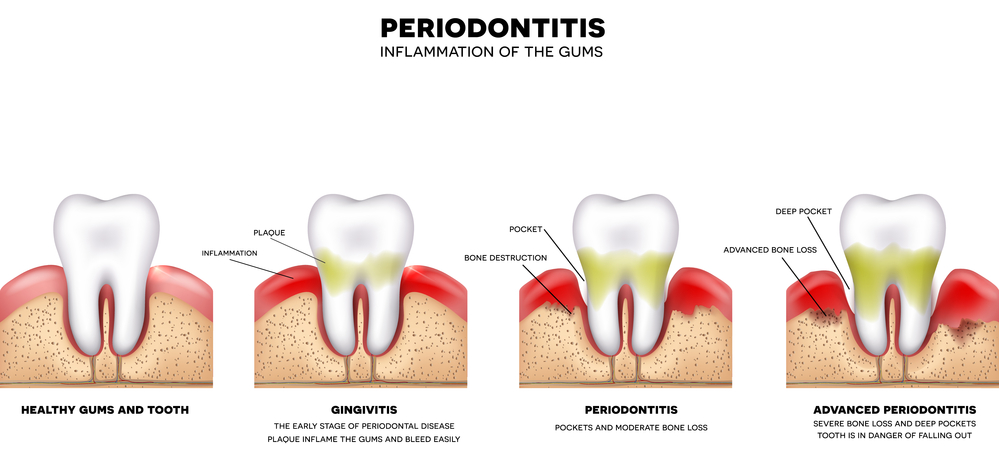
Periodontitis starts as inflammation and gets worse over time.
Inflammation (gingivitis)
Periodontitis begins with inflammation in the gums known as gingivitis. One of the first signs of gingivitis is that your gums will bleed when you brush or floss your teeth.
You might also notice some discoloration on your teeth. This is called plaque. Plaque is a buildup of bacteria and food debris on your teeth. Although bacteria are always present in your mouth, they only become harmful when conditions allow them to increase dramatically. This might happen if you don’t brush or floss, or get dental cleanings on a regular basis.
Early periodontal disease
In the early stages of periodontitis, your gums recede, or pull away, from your teeth and small pockets form between gums and teeth. The pockets harbor harmful bacteria. Your immune system tries to fight the infection, and your gum tissue starts to recede. You’ll likely experience bleeding during brushing and flossing as well, and possibly some bone loss.
Moderate periodontal disease
If left to progress to moderate periodontal disease, you might experience bleeding and pain around the teeth and gum recession. Your teeth will begin to lose bone support and become loose. The infection can also lead to an inflammatory response throughout your body.
Advanced periodontal disease
In advanced disease, the connective tissue that holds your teeth in place begins to deteriorate. The gums, bones, and other tissue that support your teeth are destroyed. If you have advanced periodontitis, you might experience severe pain while chewing, severe bad breath, and a foul taste in your mouth. You’ll likely lose your teeth.
What are the symptoms of periodontitis?
The symptoms depend on the stage of disease, but generally include:
- gums that bleed when you brush your teeth or floss
- bad breath
- changes in the position of your teeth or loose teeth
- receding gums
- red, tender, or swollen gums
- buildup of plaque or tartar on your teeth
- pain when chewing
- tooth loss
- foul taste in your mouth
- inflammatory response throughout your body
Symptoms in the early stages of periodontitis are often not very noticeable. Your dentist will likely be the first to point them out.
What causes periodontitis?
Healthy people normally have hundreds of different types of bacteria in their mouth. Most of them are completely harmless. When you don’t clean your teeth properly each day, the bacteria grow and build up on your teeth.
Periodontitis is typically caused by poor dental hygiene. When you don’t brush your teeth and clean in hard-to-reach places in your mouth, the following happens:
- The bacteria in your mouth multiply and form a substance known as dental plaque.
- If you don’t remove the plaque by brushing, the bacteria deposit minerals within the plaque over time.
- This mineral deposit is known as tartar, which will encourage more bacterial growth toward the root of the tooth.
- Your body’s immune response to this bacterial growth leads to inflammation in your gums.
- The attachment of the gum to the root of a tooth is disrupted over time, and a periodontal pocket (gap) may form between the gum and root.
- Harmful anaerobic bacteria colonize in the pocket and multiply, releasing toxins that can damage the gums, teeth, and supporting bone structures.
Additionally, certain factors put you at a higher risk of periodontitis, including:
- smoking, which is one of the biggest risk factors for periodontitis
- type 2 diabetes
- obesity
- hormonal changes in women (such as when menstruation, pregnancy, or menopause occurs), which can make the gums more sensitive
- conditions that impact your immune system, like HIVor leukemia
- medications that reduce the flow of saliva in your mouth
- genetics
- poor nutrition, including a deficiency in vitamin C
What are the complications of periodontitis?
If not treated for periodontitis, the supporting structures of your teeth, including the bones of your jaw, can be destroyed. Your teeth loosen and might fall out or require extraction. Other complications of periodontitis include:
- painful abscesses
- migration of your teeth, which may interfere with eating
- receding gums and exposure of the roots of your teeth
- increased risk of complications during pregnancy, including low birth weight and preeclampsia
- increased risk of heart disease, respiratory disease, and diabetes
How is periodontitis diagnosed?
Your dentist will be able to detect signs of periodontitis at an early stage during a routine dental examination. They can monitor your periodontal status over time to make sure it doesn’t get any worse. This is why it’s important that you visit a dentist on a regular basis for a screening.
Your dentist may use a tiny ruler called a probe to measure any pockets on your gums. This test is usually painless. If plaque, tartar, or both are found on your teeth, your dentist will remove these substances as part of a professional cleaning. They may also take dental X-rays or refer you to a periodontist, an expert in the diagnosis and treatment of gum disease, for further testing and treatment.
How is periodontitis treated?
Treatment is aimed at removing plaque and bacterial deposits on your teeth and gums.
Oral hygiene practices
Your dental care team will give you instructions on how to reduce the number of bacteria in your mouth, which involves keeping your teeth and gums clean. Your dentist will give you advice on how to use tooth brushes and dental floss properly, and may recommend other oral hygiene products like a water pick or mouthwash.
Here are a few tips for keeping your teeth healthy:
- Brush your teeth twice a day with a fluoride toothpaste.
- Consider using an electric toothbrush, which may be more effective.
- Floss at least once a day to remove plaque.
- Visit your dentist at least twice a year for a professional cleaning.
- Don’t smoke or chew tobacco.
Professional cleanings
During a professional cleaning, your dentist will remove plaque buildup and tartar from your teeth and their roots, and then polish your teeth and treat them with fluoride. Any periodontal pockets that have formed could require deep cleaning to enable healing. A deep-cleaning method called scaling and root planing will help scrape off tartar and also remove any rough spots on the tooth root where bacteria tend to gather.
Antibiotics
In some cases, your dentist will prescribe antibiotics to help with persistent gum infections that haven’t responded to cleanings. The antibiotic might be in the form of a mouthwash, gel, or an oral tablet or capsule.
Follow-up appointments
Your dentist will want to follow up with you after a few weeks, and then about every three to six months after that to assess your progress. If periodontal pockets are still present, they may recommend other treatment options, like surgery.
Surgery
If inflammation persists in sites that are inaccessible to brushing and flossing, your dentist may recommend a surgical procedure called flap surgery to clean deposits under your gums. Under anesthesia, your gums are lifted away and the roots of your teeth cleaned. Your gums are then sutured (stitched) back into place.
If you’ve had any bone loss, a procedure known as bone grafting may be done at the same time as flap surgery to regenerate the lost bone.
What is the outlook for periodontitis?
Periodontitis can be stopped if caught and treated early enough. Treatment is typically very successful.
If you have periodontitis, regular follow-ups with a dentist are essential to ensure that the disease doesn’t continue. You’ll have to change your dental hygiene habits and cooperate fully with your dentist’s instructions for a positive outcome. The long-term outlook depends on your own efforts with oral hygiene and the ongoing assessment of your dentist.
In addition to periodontitis progressing much faster in smokers, these people often have a poor outlook with periodontitis. The vast majority of cases that don’t respond to treatment involve smokers.